Tretinoin
Tretinoin treats acne. Can also reduce fine facial wrinkles. Can increase your chances of getting sunburned, so use sunscreens and wear protective clothing during treatment.
Tretinoin Overview
Tretinoin topical is a prescription medication used to reduce fine facial wrinkles or to control acne. Tretinoin is also used to treat acute promyelocytic leukemia (APL).
Tretinoin belongs to a group of drugs called retinoids. It is not known exactly how it works to reduce fine facial wrinkles. For cancer, tretinoin slows or stops the growth of cancer cells by causing immature blood cells to develop into normal blood cells.
Tretinoin topical comes in cream, gel, and topical solution forms and is applied to the face once a day.
Tretinoin also comes as a capsule to take by mouth. It is usually taken twice a day for up to 90 days. Take tretinoin at around the same times every day.
Common side effects of tretinoin topical include peeling, dry skin, and redness of the skin.
Common side effects of tretinoin capsules include headache, fever, weakness, and fatigue. Do not drive or operate heavy machinery until you know how this medication affects you.
How was your experience with Tretinoin?
Tretinoin Cautionary Labels


Uses of Tretinoin
Topical:
Tretinoin topical is a prescription medication that may reduce fine wrinkles It is for patients who are using a total skin care and sunlight avoidance program. Tretinoin does not remove wrinkles or repair sun-damaged skin. Some formulations are indicated to control acne, but does it cure acne.
This medication may be prescribed for other uses. Ask your doctor or pharmacist for more information.
Oral:
Tretinoin is used to treat acute promyelocytic leukemia (APL) in people who have not been helped by other types of chemotherapy or whose condition has improved but then worsened following treatment with other types of chemotherapy. APL is a type of cancer in which there are too many immature blood cells in the blood and bone marrow. Tretinoin is used to produce remission (a decrease or disappearance of signs and symptoms of cancer) of APL, but other medications must be used after treatment with tretinoin to prevent cancer from returning.
This medication may be prescribed for other uses. Ask your doctor or pharmacist for more information.
Tretinoin Brand Names
Tretinoin Drug Class
Tretinoin is part of the drug class:
Side Effects of Tretinoin
Topical:
Common side effects of tretinoin include peeling, dry skin, redness of the skin, burning, stinging, and itching.
This is not a complete list of tretinoin side effects. Ask your doctor or pharmacist for more information.
Tell your doctor if you have any side effect that bothers you or that does not go away.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Oral:
Common side effects of tretinoin capsules include the following:
- headache
- fever
- fatigue
- weakness
- extreme tiredness
- shivering
- pain
- earache
- feeling of fullness in the ears
- dry skin
- rash
- hair loss
- constipation
- diarrhea
- stomach pain
- heartburn
- loss of appetite
- weight loss
- bone pain
- dizziness
- numbness, burning, or tingling in the hands or feet
- nervousness
- depression
- difficulty falling asleep or staying asleep
- confusion
- agitation
- hallucinating (seeing things or hearing voices that do not exist)
- difficulty urinating
- flushing
This is not a complete list of tretinoin side effects. Ask your doctor or pharmacist for more information.
Tell your doctor if you have any side effect that bothers you or that does not go away.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Tretinoin Interactions
Topical/Oral:
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Especially tell your doctor if you take:
- thiazide diuretics
- tetracycline antibiotics such as demeclocycline (Declomycin), doxycycline (Monodox, Vibramycin, others), minocycline (Minocin), oxytetracycline (Terramycin), and tetracycline (Sumycin, Tetrex, others)
- fluoroquinolone antibiotics
- ketoconazole (Nizoral)
- phenothiazine medications
- sulfonamide-containing medications
- aminocaproic acid (Amicar)
- certain calcium channel blockers such as diltiazem (Cardizem, Dilacor, Tiazac, others) and verapamil (Calan, Covera, Isoptin, Verelan)
- cimetidine (Tagamet)
- cyclosporine (Sandimmune, Gengraf, Neoral)
- erythromycin (E.E.S., Erythrocin, E-Mycin)
- hydroxyurea (Droxia)
- pentobarbital
- phenobarbital
- rifampin (Rifadin, Rimactane)
- oral steroids such as dexamethasone (Decadron, Dexone), methylprednisolone (Medrol), and prednisone (Deltasone)
- tranexamic acid (Cyklokapron)
- vitamin A
This is not a complete list of all drug interactions. Ask your doctor or pharmacist for more information.
Topical:
You should avoid using skin products that can dry or irritate your skin because skin dryness and irritation are increased with tretinoin topical. Skin products that can dry and irritate your skin include:
- products that contain alcohol, astringents, or spices
- acne medicines that contain benzoyl peroxide, sulfur, resorcinol, or salicylic acid
- medicated soap or skin cleansers
This is not a complete list of all drug interactions. Ask your doctor or pharmacist for more information.
Tretinoin Precautions
Topical/Oral:
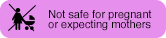
Do not use tretinoin if:
- you are pregnant or plan to become pregnant
- you are sunburned or your skin is irritated
- you are highly sensitive to sunlight
- have eczema or other skin conditions
- you are allergic to any of the ingredients in the tretinoin formulations
Topical:
- Exposure to sunlight (including sunlamps) should be avoided or minimized during use of tretinoin topical use because of heightened sunburn susceptibility.
- Tretinoin has been reported to cause severe irritation to patients with eczema and should be used only with caution if you have this particular skin condition.
- Avoid contact with the eyes, ears, nostrils, angles of the nose, and mouth. Tretinoin topical may cause severe redness, itching, burning, stinging, and peeling if used on these areas.
- Avoid excessive exposure to wind or cold. Extremes of climate tend to dry or burn normal skin. Skin treated with tretinoin may be more vulnerable to these extremes. Your physician can recommend ways to manage your acne treatment under such conditions.
Oral:
Tretinoin may cause severe side effects.
- Tretinoin may increase the levels of cholesterol and other fats in your blood and may stop your liver from working normally. Your doctor will monitor you carefully to see whether you are experiencing either of these side effects.
- Tretinoin should be given only under the supervision of a doctor who has experience in treating people who have leukemia (cancer of the white blood cells) and in a hospital where patients can be monitored for severe side effects and treated if these side effects occur.
- Tretinoin may cause a serious or life-threatening group of symptoms called retinoic acid-APL(RA-APL) syndrome. Your doctor will monitor you carefully to see whether you are developing this syndrome. If you experience any of the following symptoms, call your doctor immediately: fever; weight gain; swelling of the arms, hands, feet, ankles, or lower legs; shortness of breath; labored breathing; wheezing; chest pain; or cough. At the first sign that you are developing RA-APL syndrome, your doctor will prescribe one or more medications to treat the syndrome.
- Tretinoin may cause a rapid increase in the number of white blood cells in the body. This is associated with a higher risk of life-threatening side effects. If you have a very high number of white blood cells before you begin tretinoin treatment, or if you have an increase in the number of white blood cells during your treatment with tretinoin, especially if you experience any of the symptoms of RA-APL syndrome, your doctor may prescribe one or more medications to treat or prevent the increase in white blood cells.
- For female patients:
- Tretinoin must not be taken by patients who are pregnant or who may become pregnant. There is a high risk that tretinoin will cause the baby to be born with birth defects (physical problems that are present at birth).
- If you can become pregnant, you will need to avoid pregnancy during your treatment with tretinoin. You must use two acceptable forms of birth control during your treatment and for 1 month after your treatment, even if you have infertility (difficulty becoming pregnant) or have experienced menopause ('change of life'; end of monthly menstrual periods). You must use these two forms of birth control at all times unless you can promise that you will not have any sexual contact with a male for 1 month after your treatment. Your doctor will tell you which forms of birth control are acceptable, and will give you full information about birth control.
- If you plan to use oral contraceptives (birth control pills) while taking tretinoin, tell your doctor the name of the pill you will use. Microdosed progestin ('minipill') oral contraceptives (Ovrette, Micronor, Nor-D) may not be an effective form of birth control for people who are taking tretinoin.
- You must have a negative pregnancy test within 1 week before you begin to take tretinoin. You will also need to be tested for pregnancy in a laboratory each month during your treatment.
- Do not drive or operate heavy machinery until you know how this medication affects you.
Tretinoin Food Interactions
Topical:
Medications can interact with certain foods. In some cases, this may be harmful and your doctor may advise you to avoid certain foods. In the case of this medication, there are no specific foods that you must exclude from your diet.
Oral:
Grapefruit and grapefruit juice may interact with this medication and can lead to potentially dangerous effects. Discuss the use of grapefruit products with your doctor.
Inform MD
Before taking tretinoin, tell your doctor about all of your medical conditions. Especially tell your doctor if you:
- are allergic to tretinoin or to any of its ingredients
- are allergic to fish (if taking the Atralin brand of tretinoin)
- have eczema or other skin conditions
- have heart problems
- have elevated cholesterol levels
- have liver problems
- are pregnant or breastfeeding
- are using any other medicines to treat your acne. Do not use other medicines unless they are recommended by your doctor.
Tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements.
Tretinoin and Pregnancy
Topical:
- Tell your doctor if you are pregnant or plan to become pregnant.
- The FDA categorizes medications based on safety for use during pregnancy. Five categories - A, B, C, D, and X, are used to classify the possible risks to an unborn baby when a medication is taken during pregnancy.
- This medication falls into category C. Do not use tretinoin if you are pregnant or attempting to become pregnant. If you become pregnant while using tretinoin, please contact your doctor immediately.
Oral:
Tell your doctor if you are pregnant or plan to become pregnant.
The FDA categorizes medications based on safety for use during pregnancy. Five categories - A, B, C, D, and X, are used to classify the possible risks to an unborn baby when a medication is taken during pregnancy.
This medication falls into category D.
- YOU MUST NOT BECOME PREGNANT DURING TRETINOIN TREATMENT. There is an extremely high risk that a deformed baby will result if you become pregnant while taking tretinoin, in any amount, for even short periods of time. Potentially any exposed fetus (unborn baby) can be affected. There is also an increased risk of miscarriage. Premature births may also occur.
- Effective contraception (birth control) should be discussed with your doctor. Two forms of reliable contraception must be used during therapy, and must be continued for one month after tretinoin treatment has stopped. If directed by your doctor, two forms of reliable contraception must also be used simultaneously for at least one month before beginning therapy. It is recommended that you either abstain from sexual intercourse or use two reliable kinds of birth control at the same time. Birth control must be used even if you think you cannot become pregnant, unless you have had a hysterectomy.
- If you are pregnant or become pregnant while on tretinoin therapy or during the month after treatment has stopped, immediately contact your doctor to discuss the desirability of continuing the pregnancy.
Tretinoin and Lactation
Topical:
Tell your doctor if you are breastfeeding or plan to breastfeed.
It is not known if this medication crosses into human milk. Because many medications can cross into human milk and because of the possibility for serious adverse reactions in nursing infants with use of this medication, a choice should be made whether to stop nursing or stop the use of this medication. Your doctor and you will decide if the benefits outweigh the risk of using this medication.
Oral:
YOU MUST NOT TAKE TRETINOIN IF YOU ARE A NURSING MOTHER.
Tretinoin should not be taken by nursing mothers since it is not known whether it is excreted in human milk. Since many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from tretinoin, mothers should discontinue nursing prior to taking this drug.
Tretinoin Usage
Topical:
Use other acne medicines only on your doctor's advice and follow your doctor's instructions carefully. The medicines you have used in the past might cause too much redness or peeling.
What should I avoid while using tretinoin cream?
- Topical tretinoin can make your treated skin more sensitive to sunlight. Therefore, keep out of the sunlight as much as possible and do not use sunlamps. Avoid as much as possible products that can increase skin irritation, such as:
- other skin medicines
- medicated or abrasive (rough) soaps
- permanent wave solutions
- chemical hair removers or waxes
- electrolysis
- products with alcohol, spices, astringents, or lime
- cleansers, shampoos, or cosmetics with a strong drying effect
- other products that may irritate your skin
Topical tretinoin
- Follow your doctor's instructions on how to use the tretinoin formulation you were prescribed.
- First, wash with a mild soap, non-medicated soap and pat dry your skin gently with a towel.. WAIT 20 to 30 MINUTES BEFORE APPLYING MEDICATION; it is important for skin to be completely dry in order to minimize possible irritation.
- Be especially careful when applying tretinoin cream to avoid your eyes, ears, nostrils, angles of the nose, and mouth. Spread medication away from these areas when applying.Tretinoin cream may cause severe redness, itching, burning, stinging, and peeling if used on these areas.
- Do not use more medication or more often than your doctor has prescribed.Too much medication may irritate or increase the irritation of your skin, and will not give faster or better results.
- You can use a facial cream or lotion of SPF 15 or higher each morning after washing your face. Using a moisturizer is to protect the treated areas from dryness.Follow your doctor's advice because you need to use a cream or lotion that will not make your acne worse. Using sunscreen and wearing protective clothing will protect the treated areas from sunlight. If you sunburn easily, or if you spend a lot of time exposed to sunlight, be especially careful to protect your skin.
- You may use cosmetics one hour after applying tretinoin cream or gel. However, clean your face before using cosmetics and remove cosmetics from your skin before using this medication. Talk to your doctor about recommended cosmetics.
- You may not see improvement right away.
- Once your acne is under control you should continue to use gel as your doctor instructs you to do.
- Gels are flammable. Keep away from heat and flame.
While on tretinoin:
- Avoid frequent washings and harsh scrubbing. Acne isn't caused by dirt, so no matter how hard you scrub, you can't wash it away. Washing too frequently or scrubbing too roughly may at times actually make your acne worse. Wash your skin gently with a mild, bland soap. Two or three times a day should be sufficient. Pat skin dry with a towel. Remember, excessive irritation such as rubbing, too much washing, use of other medications not suggested by your physician, etc., may worsen your acne.
- Renova (tretinoin cream)
- Use tretinoin cream as a part of a total skin care and sun avoidance program. Tretinoin cream is usually applied to the face once a day in the evening.
- Squeeze a small amount of tretinoin cream on your fingertip, and apply to your face. This looks about the size of a pearl about ¼ inch or 5mm diameter. This should be enough to cover your affected area lightly.
- Use tretinoin cream as a part of a total skin care and sun avoidance program. Tretinoin cream is usually applied to the face once a day in the evening.
- Retin-A (tretinoin cream, gel, or topical solution)
- Apply medication daily before bedtime, or as directed by your physician. Your physician may advise, especially if your skin is sensitive, that you start your therapy by applying medication every other night.
- Cream and Gel: Squeeze about a half inch or less of medication onto the fingertip. While that should be enough for your whole face, after you have some experience with the medication you may find you need slightly more or less to do the job. The medication should become invisible almost immediately. If it is still visible, or if dry flaking occurs from the gel within a minute or so, you are using too much. Cover the affected area lightly with cream or gel by first dabbing it on your forehead, chin and both cheeks, then spreading it over the entire affected area. Smooth gently into the skin.
- Topical Solution: Retin-A topical solution may be applied to the skin where acne lesions appear, spreading the medication over the entire affected area, using a fingertip, gauze pad, or cotton swab. If gauze or cotton is employed, care should be taken not to oversaturate it to the extent that the solution would run into areas where treatment is not intended (such as corners of the mouth, eyes, and nose).
- Retin-A Microspheres (tretinoin gel)
- Apply gel once a day in the evening, or as directed by your doctor.
- Squeeze a small amount of gel (about the size of a pea) on your fingertip. Dab gel on your forehead, chin, and both cheeks. Spread medication evenly over the entire surface of your face by gently smoothing it into your skin.
- Avita (tretinoin cream or gel)
- Cream or gel should be applied once a day, in the evening, or as directed by your physician, to the skin where acne lesions appear, using enough to cover the entire affected area lightly.
- Squeeze about a half inch or less of medication onto the fingertip. While that should be enough for your whole face, after you have had some experience with the medication you may find you need slightly more or less to do the job. The medication should become invisible almost immediately. If it is still visible, or if dry flaking occurs from the gel within a minute or so you are using too much. Cover the affected area lightly with medication by first dabbing it on your forehead, chin, and both cheeks, then spreading it over the entire affected area. Smooth gently into the skin.
- Atralin (tretinoin gel):
- Apply gel once a day before bedtime.
- Squeeze a small amount of gel (about the size of a pea) on your fingertip. Apply gel, using a thin layer to cover the entire affected area. Smooth gel gently into your skin.
Oral:
Tretinoin comes as a capsule to take by mouth. It is usually taken twice a day for up to 90 days. Take tretinoin at around the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take tretinoin exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Continue to take tretinoin even if you feel well. Do not stop taking tretinoin without talking to your doctor.
Tretinoin Dosage
Topical:
- Renova (tretinoin)- Apply a small pearl-sized (about ¼ inch or 5 millimeter diameter) amount of cream to cover the entire affected area lightly. Caution should be taken when applying the cream to avoid the eyes, ears, nostrils, and mouth.
- Retin-A (tretinoin) - Use enough to cover the entire affected area lightly.
- Avita (tretinoin) - Squeeze about a half inch or less of medication onto the fingertip. While that should be enough for your whole face, after you have had some experience with the medication you may find you need slightly more or less to do the job.
- Atralin (tretinoin) - Use a thin layer to cover the entire affected area.
Oral:
The recommended dose is 45 mg/m2/day given as two evenly divided doses until complete remission is documented.
Tretinoin Overdose
If you take too much this medication, call your healthcare provider or local Poison Control Center, or seek emergency medical attention right away.
If this medication is administered by a healthcare provider in a medical setting, it is unlikely that an overdose will occur. However, if an overdose is suspected, seek emergency medical attention.
Other Requirements
- Renova (tretinoin cream): store at room temperature
- Retin-A: store below 80˚F
- Retin-A microsphere: store at room temperature
- Avita: store below 86˚F
- Atralin: store at room temperature
- Tretinoin capsules: store at room temperature
Tretinoin FDA Warning
Oral:
1.Experienced Physician and Institution
Patients with acute promyelocytic leukemia (APL) are at high risk in general and can have severe adverse reactions to tretinoin. Tretinoin should therefore be administered only to patients with APL under the strict supervision of a physician who is experienced in the management of patients with acute leukemia and in a facility with laboratory and supportive services sufficient to monitor drug tolerance and protect and maintain a patient compromised by drug toxicity, including respiratory compromise. Use of tretinoin requires that the physician concludes that the possible benefit to the patient outweighs the following known adverse effects of the therapy.
2. Retinoic Acid-APL Syndrome
About 25% of patients with APL treated with tretinoin have experienced a syndrome called the retinoic-acid-APL (RA-APL) syndrome characterized by fever, dyspnea, acute respiratory distress, weight gain, radiographic pulmonary infiltrates, pleural and pericardial effusions, edema, and hepatic, renal, and multi-organ failure. This syndrome has occasionally been accompanied by impaired myocardial contractility and episodic hypotension. It has been observed with or without concomitant leukocytosis. Endotracheal intubation and mechanical ventilation have been required in some cases due to progressive hypoxemia, and several patients have expired with multi-organ failure. The syndrome generally occurs during the first month of treatment, with some cases reported following the first dose of tretinoin.
The management of the syndrome has not been defined rigorously, but high dose steroids given at the first suspicion of the RA-APL syndrome appear to reduce morbidity and mortality. At the first signs suggestive of the syndrome (unexplained fever, dyspnea and/or weight gain, abnormal chest auscultatory findings or radiographic abnormalities), high dose steroids (dexamethasone 10 mg intravenously administered every 12 hours for 3 days or until the resolution of symptoms) should be immediately initiated, irrespective of the leukocyte count. The majority of patients do not require termination of tretinoin therapy during treatment of the RA-APL syndrome. However, in cases of moderate and severe RA-APL syndrome, temporary interruption of tretinoin therapy should be considered. 1
3.Leukocytosis at Presentation and Rapidly Evolving Leukocytosis During Tretinoin Treatment
During tretinoin treatment about 40% of patients will develop rapidly evolving leukocytosis. Patients who present with high WBC at diagnosis (> 5x109/L) have an increased risk of a further rapid increase in WBC counts. Rapidly evolving leukocytosis is associated with a higher risk of life threatening complications.
If signs and symptoms of the RA-APL syndrome are present together with leukocytosis, treatment with high dose steroids should be initiated immediately. Some investigators routinely add chemotherapy to tretinoin treatment in the case of patients presenting with a WBC count of > 5x109/L or in the case of a rapid increase in WBC count for patients leukopenic at start of treatment, and have reported a lower incidence of the RA-APL syndrome. Consideration could be given to adding full dose chemotherapy (including an anthracycline if not contraindicated) to the tretinoin therapy on day 1 or 2 for patients presenting with a WBC count of > 5x109/L, or immediately, for patients presenting with a WBC count of < 5x109/L, if the WBC count reaches ≥ 6x109/L by day 5, or ≥ 10x109/L by day 10, or ≥ 15x109/L by day 28.
4.Teratogenic Effects. Pregnancy Category D
There is a high risk that a severely deformed infant will result if tretinoin is administered during pregnancy. If, nonetheless, it is determined that tretinoin represents the best available treatment for a pregnant woman or a woman of childbearing potential, it must be assured that the patient has received full information and warnings of the risk to the fetus if she were to be pregnant and of the risk of possible contraception failure and has been instructed in the need to use two reliable forms of contraception simultaneously during therapy and for 1 month following discontinuation of therapy, and has acknowledged her understanding of the need for using dual contraception, unless abstinence is the chosen method.
Within 1 week prior to the institution of tretinoin therapy, the patient should have blood or urine collected for a serum or urine pregnancy test with a sensitivity of at least 50 mIU/mL. When possible, tretinoin therapy should be delayed until a negative result from this test is obtained. When a delay is not possible, the patient should be placed on two reliable forms of contraception. Pregnancy testing and contraception counseling should be repeated monthly throughout the period of tretinoin treatment.