Teriparatide
Teriparatide treats those with osteoporosis. It is injected just under the skin of the stomach area or thigh once a day. It is best to rotate injection sites.
Teriparatide Overview
Teriparatide is a prescription medication used to treat both men and postmenopausal women with osteoporosis who are at high risk for having broken bones. Teriparatide is a synthetic hormone that is similar to the one the body makes naturally (parathyroid hormone). It works by causing the body to build new bone and increase bone strength by regulating calcium and phosphate.
Teriparatide comes in an injectable form that is given once daily. It is injected just under the skin of the stomach area or thigh.
Common side effects include nausea, joint aches, and pain.
How was your experience with Teriparatide?
Teriparatide Cautionary Labels


Uses of Teriparatide
Teriparatide is a prescription medication used to treat both men and postmenopausal women with osteoporosis who are at high risk for having broken bones.
This medication may be prescribed for other uses. Ask your doctor or pharmacist for more information.
Teriparatide Brand Names
Teriparatide Drug Class
Teriparatide is part of the drug class:
Side Effects of Teriparatide
Teriparatide can cause serious side effects including:
- Decrease in blood pressure when you change positions. Some people feel dizzy, get a fast heartbeat, or feel faint right after the first few doses. This usually happens within 4 hours of taking teriparatide and goes away within a few hours.
- For the first few doses, take your injections of teriparatide in a place where you can sit or lie down right away if you get these symptoms. If your symptoms get worse or do not go away, stop taking teriparatide and call your healthcare provider.
- Increased calcium in your blood. Tell your healthcare provider if you have nausea, vomiting, constipation, low energy, or muscle weakness. These may be signs there is too much calcium in your blood.
Common side effects of teriparatide include:
- nausea
- joint aches
- pain
Your healthcare provider may take samples of blood and urine during treatment to check your response to teriparatide. Also, your healthcare provider may ask you to have follow-up tests of bone mineral density.
Teriparatide Interactions
Tell your healthcare provider about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements. Your healthcare provider needs this information to help keep you from taking teriparatide with other medicines that may harm you. Especially tell your doctor if you take medicines that contain digoxin (Digoxin, Lanoxicaps, Lanoxin).
Teriparatide Precautions
- During the drug testing process, the medicine in teriparatide caused some rats to develop a bone cancer called osteosarcoma. In people, osteosarcoma is a serious but rare cancer. Osteosarcoma has been reported rarely in people who took teriparatide. It is not known if people who take teriparatide have a higher chance of getting osteosarcoma.
- You should not take teriparatide for more than 2 years over your lifetime.
- There is a voluntary Patient Registry for people who take teriparatide. The purpose of the registry is to collect information about the possible risk of osteosarcoma in people who take teriparatide.
Do not use teriparatide if you are allergic to any of the ingredients in teriparatide.
Teriparatide Food Interactions
Medicines can interact with certain foods. In some cases, this may be harmful and your doctor may advise you to avoid certain foods. In the case of teriparatide there are no specific foods that you must exclude from your diet when receiving teriparatide.
Inform MD
Tell your doctor if you are allergic to any of the ingredients in teriparatide.
Before you take teriparatide, tell your healthcare provider if you:
- have Paget's disease or other bone disease
- have cancer in your bones
- have trouble injecting yourself and do not have someone who can help you
- are a child or young adult whose bones are still growing
- have or have had kidney stones
- have had radiation therapy
- have or had too much calcium in your blood
- have any other medical conditions
- are pregnant or thinking about becoming pregnant. It is not known if teriparatide will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if teriparatide passes into your breast milk. You and your doctor should decide if you will take teriparatide or breastfeed. You should not do both.
Tell your healthcare provider about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements. Your healthcare provider needs this information to help keep you from taking teriparatide with other medicines that may harm you. Especially tell your doctor if you take medicines that contain digoxin (Digoxin, Lanoxicaps, Lanoxin).
Teriparatide and Pregnancy
Tell your doctor if you are pregnant or plan to become pregnant.
The FDA categorizes medications based on safety for use during pregnancy. Five categories - A, B, C, D, and X, are used to classify the possible risks to an unborn baby when a medication is taken during pregnancy.
This medication falls into category C. In animal studies, pregnant animals were given this medication and had some babies born with problems. No well-controlled studies have been done in humans. Therefore, this medication may be used if the potential benefits to the mother outweigh the potential risks to the unborn child.
Teriparatide and Lactation
Tell your doctor if you are breastfeeding or planning to breastfeed. It is not known if teriparatide is excreted in human breast milk or if it will harm your nursing baby.
Teriparatide Usage
- Inject teriparatide one time each day in your thigh or abdomen (lower stomach area). Talk to a healthcare provider about how to rotate injection sites.
- Before you try to inject teriparatide yourself, a healthcare provider should teach you how to use the teriparatide delivery device to give your injection the right way.
- You can take teriparatide with or without food or drink.
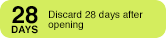
- The teriparatide delivery device has enough medicine for 28 days. It is set to give a 20 microgram dose of medicine each day. Do not inject all the medicine in the teriparatide delivery device at any one time.
- Do not transfer the medicine from the teriparatide delivery device to a syringe. This can result in taking the wrong dose of teriparatide. If you do not have pen needles to use with your teriparatide delivery device, talk with your healthcare provider.
- Teriparatide should look clear and colorless. Do not use teriparatide if it has particles in it, or if it is cloudy or colored.
- Inject teriparatide right away after you take the delivery device out of the refrigerator.
- After each use, safely remove the needle, recap the delivery device, and put it back in the refrigerator right away.
- You can take teriparatide at any time of the day. To help you remember to take teriparatide, take it at about the same time each day.
- If you forget or can not take teriparatide at your usual time, take it as soon as you can on that day. Do not take more than one injection in the same day.
- If you take more teriparatide than prescribed, call your healthcare provider. If you take too much teriparatide, you may have nausea, vomiting, weakness or dizziness.
- Follow your healthcare provider's instructions about other ways you can help your osteoporosis, such as exercise, diet, and reducing or stopping your use of tobacco and alcohol. If your healthcare provider recommends calcium and vitamin D supplements, you can take them at the same time you take teriparatide.
Teriparatide Dosage
The recommended teriparatide dose is 20 mcg given subcutaneously once a day. Your doctor will determine the best dose for you. Take teriparatide exactly as prescribed by your doctor. Follow the directions on your prescription label carefully.
Teriparatide Overdose
If you take too much teriparatide, call your healthcare provider or local Poison Control Center, or seek emergency medical attention right away.
If teriparatide is administered by a healthcare provider in a medical setting, it is unlikely that an overdose will occur. However, if overdose is suspected, seek emergency medical attention.
Other Requirements
- Keep your teriparatide delivery device in the refrigerator between 36° to 46°F (2° to 8°C).
- Do not freeze the teriparatide delivery device. Do not use teriparatide if it has been frozen.
- Do not use teriparatide after the expiration date printed on the delivery device and packaging.
- Throw away the teriparatide delivery device after 28 days even if it has medicine in it (see the User Manual). Keep teriparatide and all medicines out of the reach of children.
Teriparatide FDA Warning
WARNING: POTENTIAL RISK OF OSTEOSARCOMA
In male and female rats, teriparatide caused an increase in the incidence of osteosarcoma (a malignant bone tumor) that was dependent on dose and treatment duration. The effect was observed at systemic exposures to teriparatide ranging from 3 to 60 times the exposure in humans given a 20-mcg dose. Because of the uncertain relevance of the rat osteosarcoma finding to humans, prescribe teriparatide only for patients for whom the potential benefits are considered to outweigh the potential risk. Teriparatide should not be prescribed for patients who are at increased baseline risk for osteosarcoma (including those with Paget's disease of bone or unexplained elevations of alkaline phosphatase, pediatric and young adult patients with open epiphyses, or prior external beam or implant radiation therapy involving the skeleton) [see Warnings and Precautions, Adverse Reactions, and Nonclinical Toxicology.